Prediabetes is linked to heart attacks
Research presented at the recently completed 2022 conference of the Endocrine Society and reported in MDedge / Cardiology adds to the massive body of evidence that metabolic health is necessary for cardiovascular health and the vital importance of attending to cardiometabolic risk factors.
“Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.””
Evidence already established for prediabetes and cardiovascular disease
In Association between prediabetes and risk of all cause mortality and cardiovascular disease: updated meta-analysis published in the BMJ (British Medical Journal) two years ago, prediabetes was associated with a statistically significant 16% increase in coronary heart disease and a 13% increased risk of all-cause mortality (dying from anything).
“Results indicated that prediabetes was associated with an increased risk of all cause mortality and cardiovascular disease in the general population and in patients with atherosclerotic cardiovascular disease. Screening and appropriate management of prediabetes might contribute to primary and secondary prevention of cardiovascular disease.
Considering the high prevalence of prediabetes, and the robust and significant association between prediabetes and health risk shown in our study, successful intervention in this large population could have a major effect on public health…Furthermore, the 30 year results of the Da Qing Diabetes Prevention Outcome Study showed that lifestyle intervention in people with impaired glucose tolerance reduced the incidence of cardiovascular events and all cause mortality, providing strong justification for intervention for prediabetes.39”
The increased risk was seen even when fasting plasma glucose concentrations were as low as 5.6-6.9 mmol/L, supported by a meta-analysis of individual participant data performed by the Emerging Risk Factors Collaboration, which showed that fasting plasma glucose concentrations exceeding 5.6 mmol/L [100 mg/dL] were associated with increased mortality.31…In this study, we found that the risk of composite cardiovascular events and coronary heart disease was increased in the general population with a HbA1c concentration of 39-47 mmol/mol (5.7-6.4%).
…we found that prediabetes was also associated with an increased risk of mortality and cardiovascular outcomes in patients with established atherosclerotic cardiovascular disease. These results suggest that managing prediabetes in patients with established atherosclerotic cardiovascular disease might also be an important goal to lower their future risk of recurrent cardiovascular disease and premature death.”
Prediabetes is also associated with much more frequent invasive cardiovascular interventions:
“A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.”
Call for greater awareness by clinicians
The incidence of both prediabetes and full-blown diabetes is rapidly increasing—the CDC predicts that 38% of the adult population will have prediabetes by 2030.
“Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota.””
MDedge also quotes Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston:
““In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.””
Long recognized adverse vascular effects of prediabetes
This is not new information for cardiologists who have advanced their practice to embrace the crucial cardiometabolic component or functional medicine clinicians who as a matter of course are attentive to such associations.
In The Vasculature in Prediabetes published in Circulation Research in 2018, point out the leading roles played by insulin and inflammation in damaging the the endothelium (the living inner wall of blood vessels).
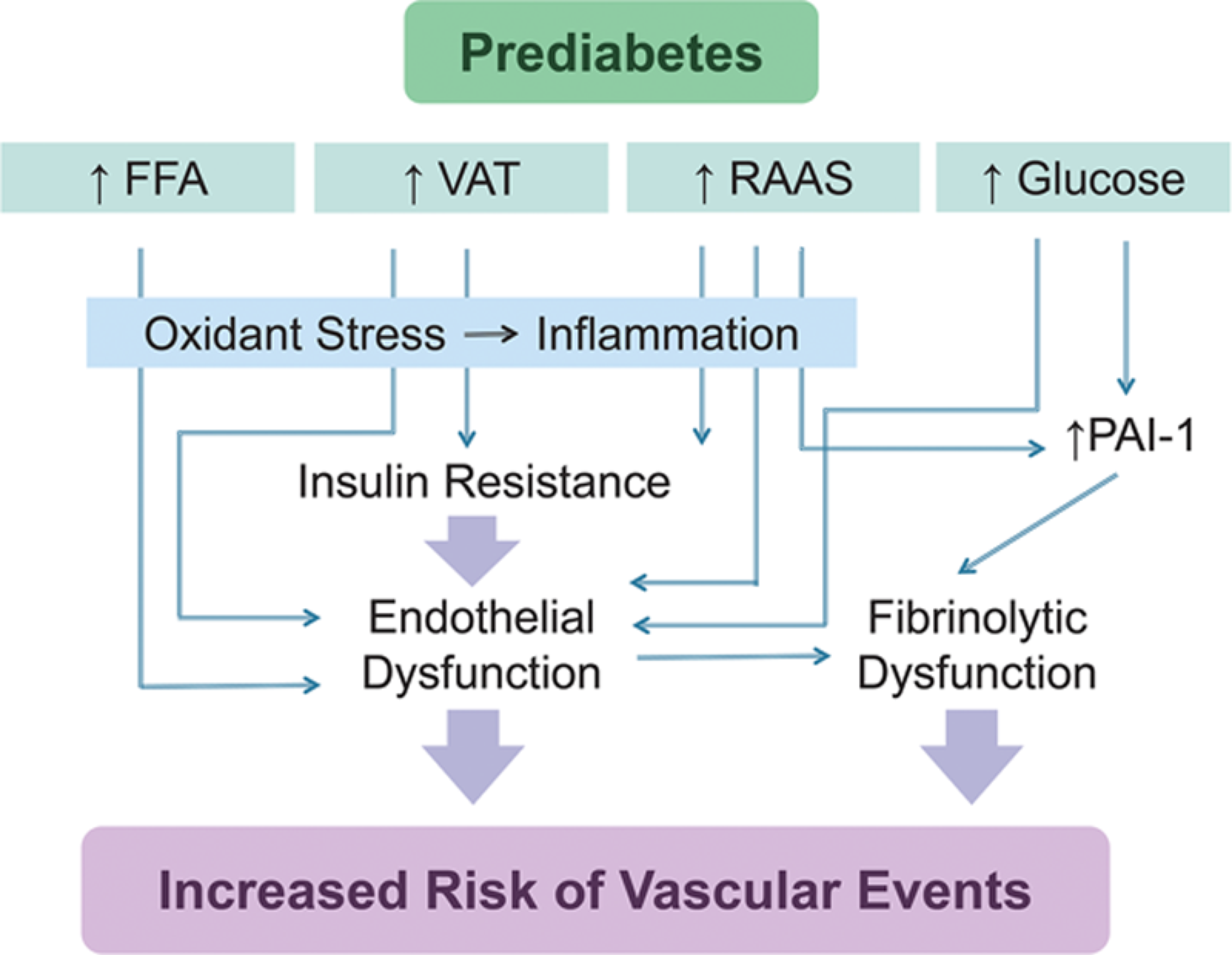
“In prediabetes, hyperglycemia, insulin resistance, and inflammation and metabolic derangements associated with concomitant obesity cause endothelial vasodilator and fibrinolytic dysfunction, leading to increased risk of cardiovascular and renal disease.”
”Prediabetes is defined clinically by hyperglycemia. Pathophysiologic features include vascular insulin resistance, oxidative stress, and inflammation, which collectively promote endothelial vasodilator and fibrinolytic dysfunction. Concomitant obesity increases inflammation and free fatty acids to exacerbate these processes.”
Endothelial insulin resistance, hyperglycemia and the formation of advanced glycation products, and increased free fatty acids (FFAs) give rise to oxidative stress, inflammation and endothelial vasodilator, and fibrinolytic dysfunction in prediabetes. PAI-1 indicates plasminogen activator inhibitor-1; RAAS renin–angiotensin–aldosterone system; and VAT, visceral adipose tissue.
An abundance of evidence-based resources is available that help to reverse prediabetes and its associated vascular damage, especially the crucial inner lining of the blood vessel called the glycocalyx that is so vulnerable to elevated insulin and glucose.